- Oct 17, 2025
3 Things Therapists Do That Are Actually Unethical
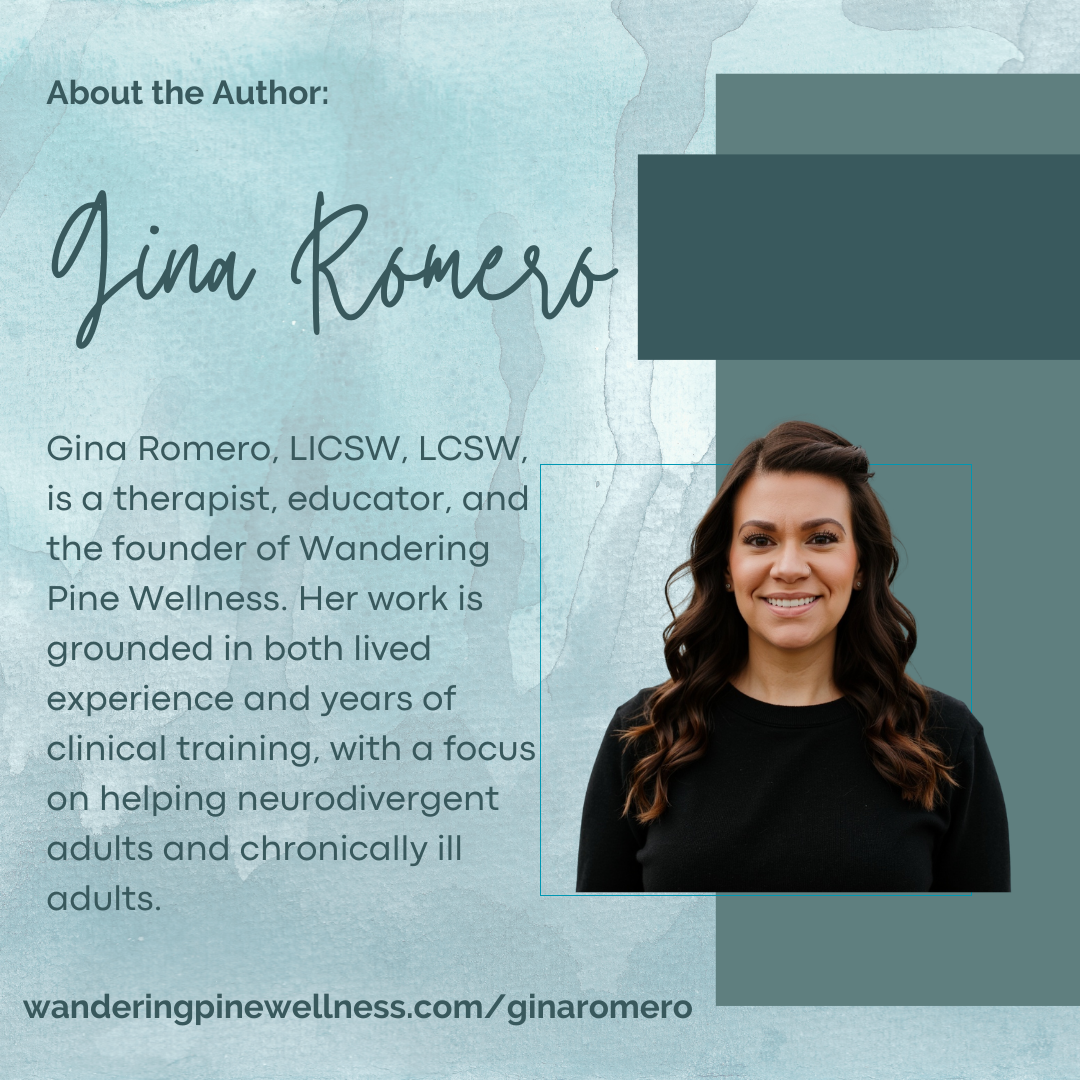
- Gina Romero
- practice management
- 0 comments
Sometimes our “standard practices” as therapists are the exact opposite of ethical; they’re just… common.
And I don’t mean the headline-grabbing stuff (dual relationships, inappropriate touch, etc.). We’re talking about the quietly unethical, the admin-level bad habits that have somehow become normalized because everyone’s busy, stressed, and trying to stay afloat under the weight of insurance panels and paperwork.
Let’s talk about three things therapists do that are 100% not okay — even though you’ve probably seen all three.
1. Ghosting Clients When Their Insurance Changes
You know the drill: your client emails you, “Hey, my insurance switched to Cigna next month. Do you take that?”
You sigh. You do, but you’ve been trying not accept new Cigna clients because the pay is too low. You respond, “I do, but I’m not accepting new Cigna clients. We’ll need to cancel your upcoming appointments.”
And that’s it.
That’s abandonment.
The APA Ethics Code (10.10) and NASW 1.17 make it crystal clear: we don’t get to disappear just because billing got complicated. Sure, you’re not obligated to keep seeing them indefinitely for free, but you are obligated to provide reasonable notice and referrals.
What Ethical Termination Actually Looks Like
Give adequate notice (not “effective immediately”). 30-60 days is recommended.
Offer a few qualified referrals.
Help them transition smoothly, especially if they’re mid-treatment or in crisis.
Document everything (because you know the one time you don’t, it’ll come back to bite you.)
Hot take: “Insurance changed” isn’t an ethical get-out-of-jail-free card. If we expect clients to navigate system chaos, we can handle a couple of bridge sessions or referral calls.
2. Accepting Payments via Personal Venmo, Zelle, or CashApp
Look, I get it. Venmo is convenient. CashApp is instant. …and Stripe takes a fee. But when you’re taking therapy payments on your personal Venmo, you’re basically saying,
“HIPAA, never heard of her.”
These platforms are not secure or not private. Personal Venmo literally lets other users see your transactions. (“$150 for depression talk 😬”)
If you have a shared bank account with a partner or family member, you risk violating your clients’ confidentiality if your partner sees the clients’ names on those transactions.
The Ethics and the Law
No Business Associate Agreement (BAA) = no HIPAA compliance.
Personal payment apps expose client identities and session frequencies.
Even if a client “doesn’t mind,” you don’t get to waive privacy laws.
A Better Solution
Use platforms like IVY Pay, SimplePractice, or TheraNest; all HIPAA-compliant and built for therapists. Or at the very least, have a business Stripe or PayPal account with a BAA on file.
Nobody should see your client’s payment showing up in your public Venmo feed between “🍕 dinner with Alex” and “💅 mani-pedi.”
3. Holding Client Records Hostage Over Unpaid Balances
This one’s surprisingly common. And honestly, it’s the ethical equivalent of “if you don’t clean your room, no dinner for you.”
You can’t withhold client records because they owe you money. You just can’t. Not legally, and not ethically.
HIPAA and every major code of ethics say clients have a right to their records. You can charge a reasonable copying fee (make sure it’s outlined clearly in your consent paperwork!), but you can’t make payment a condition of access.
Why It’s a Problem
It undermines client autonomy.
It delays or prevents continuity of care.
It puts you at risk for licensing board complaints and civil penalties.
What To Do Instead
Release the records within 30 days as required.
Charge a small administrative fee if needed.
Handle the unpaid balance through standard collection or follow-up, not by gatekeeping clinical documentation.
So Why Do These Ethical Slips Keep Happening?
Because private practice is a grind. And dealing with insurance is exhausting.
But ethical shortcuts (even tiny ones) add up. They erode client trust, damage our credibility as a profession, and make it harder to advocate for ourselves when we’re genuinely trying to do the right thing.
How to Stay Out of the Ethical Danger Zone
Review your informed consent every year. Does it still reflect your current fees, policies, and record release practices?
Use secure systems for everything: notes, payments, telehealth.
Consult before you act if something feels murky. (Seriously, 10 minutes with a colleague can save your license. And most liability insurances provide free legal consults)
Build admin buffers into your schedule. Rushed therapists make bad ethical calls.
FAQs for the Overworked, Well-Meaning Therapist
1. “But what if I can’t afford to keep seeing a client after insurance changes?”
Totally fair. You don’t have to, but you do have to plan the termination ethically. Provide notice, referrals, and documentation. You’re closing a case, not ghosting a friend.
2. “Everyone I know uses Venmo for payments. Is it really that bad?”
Yes. It’s that bad. Just because it’s common doesn’t make it compliant. “Everyone’s doing it” is how ethics complaints start.
3. “Do I need a HIPAA BAA for payment processors?”
If they touch client info (name, date, amount), yes. No BAA = no compliance.
4. “Has anyone ever actually been disciplined for this stuff?”
Absolutely. Licensing boards routinely sanction clinicians for abandonment, record access issues, and confidentiality breaches, not just major misconduct.
Moving Forward
We all fuck up sometimes. But the difference between a misstep and misconduct is how fast we correct it.
If you’re doing any of these three things ) ghosting clients after an insurance change, using personal Venmo, or withholding records) you don’t need to panic. You’re just overdue for an ethics tune-up.